Summary
- New MRI technology for non-invasive evaluation of spermatogenic potential in the testes in male infertility
- Creatine levels in the testes, which correlate with spermatogenic potential, are measured with a special MRI.
- The imaging technology provides useful information for diagnosis and treatment decisions in male infertility.
- If we establish good spatial resolution on this technology, you can improve the sperm collection rate in microscopic testicular sperm extraction
- Proposals for companies
- For MRI equipment manufacturer: New functionality for imaging creatine concentration distribution
- For Pharmaceutical company: Provision of information and joint research for the development of drugs to treat infertility
Background & Technology
We propose a new application of MRI that can help in the diagnosis of male infertility and the development of its treatment. This technology can not only evaluate the spermatogenic potential of the testes, but also visualize the areas of spermatogenesis. When the concentration distribution of creatine (a type of organic acid and known as an energy source for muscles), which is used in sperm production, is measured using a MRI technology based on chemical exchange saturation transfer (CEST-MRI), areas of high creatine concentration can be visualized as areas of high sperm production performance.
The main causes of male infertility are hypospermia (low semen volume), oligozoospermia (low sperm count) and azoospermia (no sperm in the semen). Understanding the status of testicular function is important to elucidate the causes of these conditions and to select appropriate treatment. When sperm cannot be extracted from the semen, sperm are attempted to be extracted from the testicular tissue by surgery, microscopic testicular sperm extraction (Micro TESE), but the sperm extraction rate is as low as about 30%, so a method that can visualize the area of sperm production is needed.
Dr. Hidetaka Kioka of the The University of Osaka Graduate School of Medicine, Dr. Shinichiro Fukuhara, a specialist in urology, and their colleagues have developed the new technology described above, which is expected to make a significant contribution to the formulation of treatment policies based on an understanding of the state of testicular function and to prognostic judgments before and after surgery and treatment.
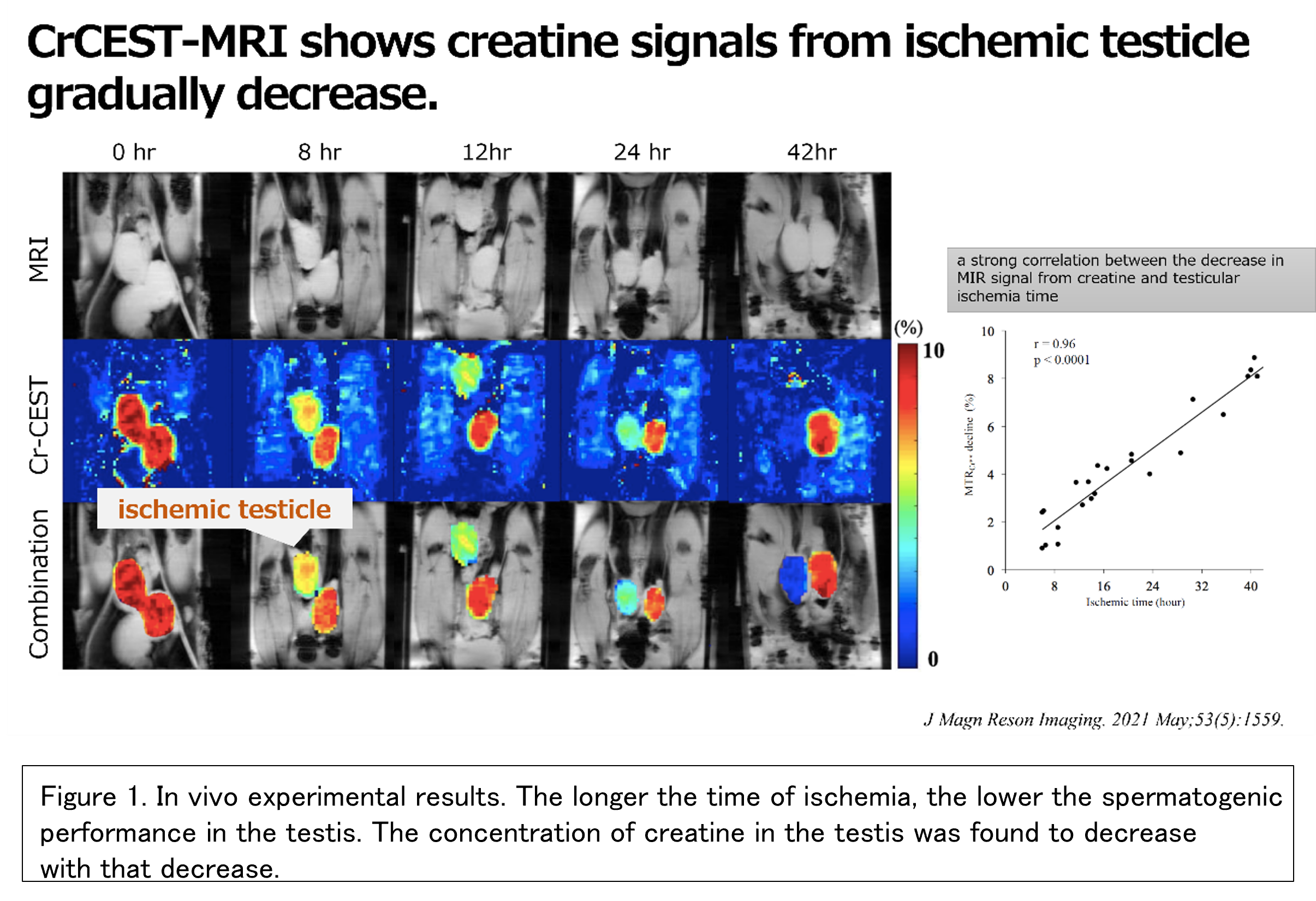
The developers have already demonstrated the technology in in vivo experiments. They applied the technology to a mouse model of testicular ischemia caused by testicular torsion or peritoneal retention and confirmed that testicular dysfunction can be detected based on creatine concentration (Fig. 1). In another experiment with mice whose testes were irradiated with X-rays, differences in creatine concentration were observed between the irradiated and non-irradiated areas.
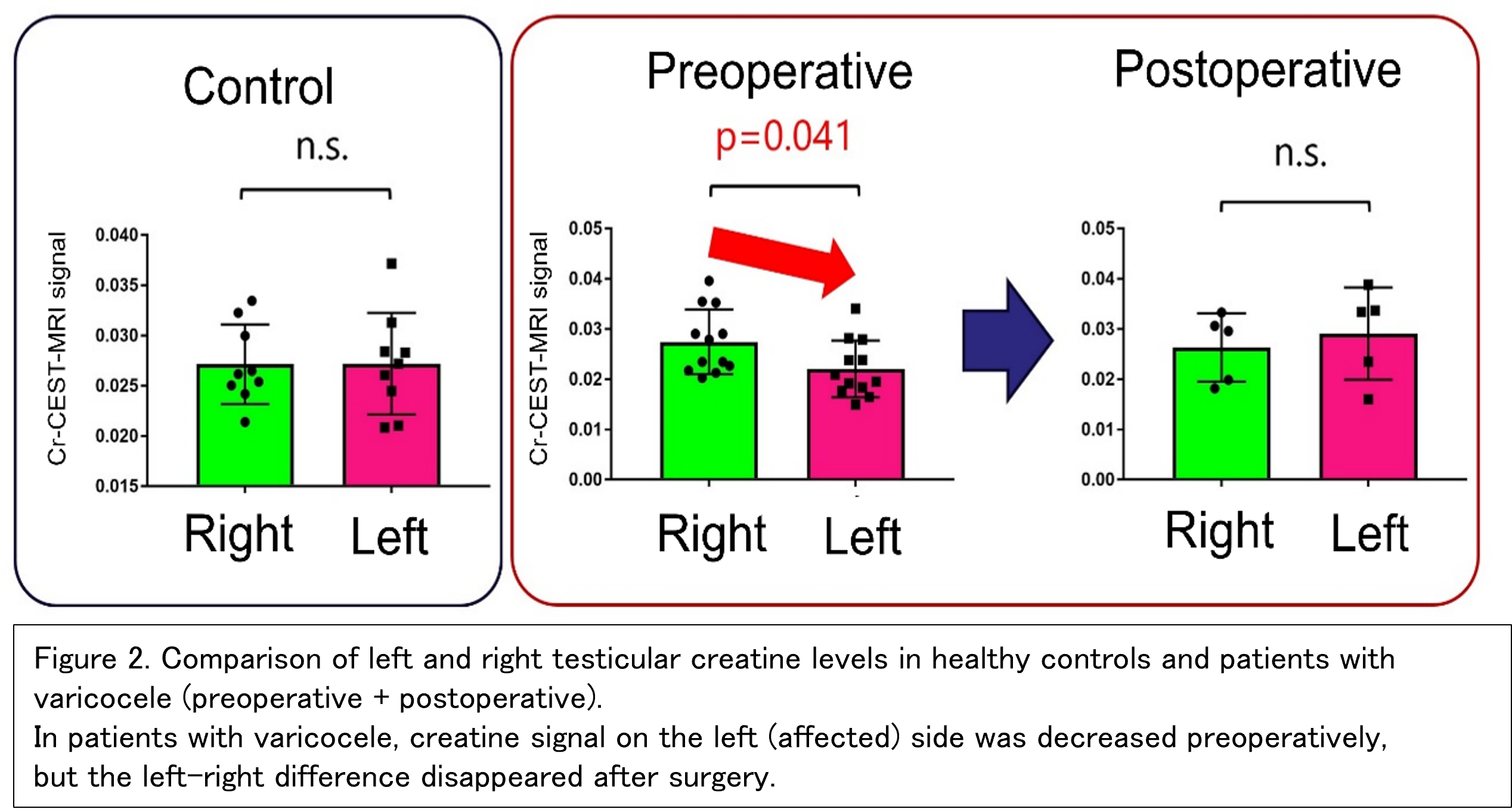
The developers have also confirmed the effectiveness of this technology in patients with varicocele, one of the main causes of male infertility. As a result of measuring creatine concentration with this technology, no difference in creatine concentration was observed between the left and right testis in healthy subjects (Figure 2, left), but in patients with varicocele, creatine concentration was decreased in the affected (left) testis (Figure 2, middle). Importantly, creatine concentration in the left testis improved after varicocele surgery and the left-right difference disappeared (Figure 2, right). This indicates that this technology accurately reflects the spermatogenic potential of the testis. At the same time, there were no abnormalities in temperature change or appearance of the testis due to the use of this technology, nor were there any complaints of abnormality from the subject, confirming the safety of this technology. Further accumulation of cases is expected to clarify the superiority of this technique in confirming the effectiveness of the surgery.
Microscopic Testicular Sperm Extraction (Micro TESE) is a procedure to extract sperm from testicular tissue for male infertility patients who are unable to extract sperm from semen, but the success rate is low at about 30%. To improve the success rate, it is essential to visualize the location of the sperm. This technology is expected to improve the sperm extraction rate of Micro TESE by visualizing the areas where sperm can potentially be extracted. Another situation in which this technology can be used is to provide information for research and development related to the development of drug treatments for male infertility. It is expected that this technology will facilitate drug development for male infertility by providing an objective index of spermatogenic potential in a simple manner.
As described above, this technology is useful for proper diagnosis, selection of appropriate treatment strategies, confirmation of surgical efficacy, improvement of the success rate of Micro TESE, and as an objective indicator of spermatogenesis in drug development, and can be used to develop new strategies to cope with the declining birthrate.
 |
 |
Researcher
Hidetaka Kioka, Assistant Professor
Shinichiro Hukuhara, Associate Professor
They are in Graduate School of Medicine / Faculty of Medicine, The University of Osaka.
Expectation
The University of Osaka is looking for companies that are willing to collaborate with the developers to establish tests and treatment methods for male infertility treatment using this technology.
- For MRI equipment manufacturer: Why don’t you incorporate this technology into your MRI equipment? We expect that this technology will further bring out the potential of your products, and will enable you to expand into new businesses and services.
- For pharmaceutical companies: Why don’t you utilize this technology for the development of drugs and treatments for male infertility? We can discuss the use of this technology within your company as well as the development of treatment technologies through joint research with The University of Osaka.
The developers have now completed a basic in vivo demonstration of the technology and are gathering insights for practical application in clinical research. The development team includes professionals with expertise in urology and MRI imaging. We would be happy to discuss specific strategies for commercialization with you, as we can provide you with details of the technology as well as needs from clinical infertility treatment by exchanging ideas with the developers.
Project.DA-03136a


