Advantages
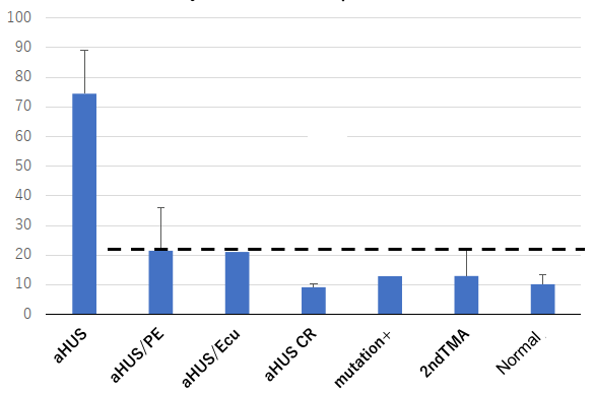
- aHUS differential diagnosis and remission monitoring, which was difficult with conventional methods, is possible.
- Responder to complement targeting drugs (anti-C5 antibodies, etc.) can be determined.
Background and Technology
Atypical hemolytic uremic syndrome (aHUS) is a type of thrombotic microangiopathy (TMA) and exhibits pathological conditions similar to secondary TMA such as collagen disease-related TMA. It differs from other TMA in that the cause is vascular endothelial cell damage due to disordered activation of genetic/acquired complement, and it is a serious disease with a high risk of maintenance dialysis and death.
The current diagnosis of aHUS is based on a combination of abnormalities in complement-related genes, the presence of anti-factor H antibodies, which are complement regulators, and clinical diagnosis. However, there are no clear criteria for diagnosis, and it is difficult to differentiate it from unsymptomatic genetic carriers and collagen disease-related TMA. The number of cases of aHUS occurring in Japan is approximately several dozen to several hundred cases per year, but the number of cases of collagen disease-related TMA, which is the subject of this differential diagnosis, is thought to be approximately 10,000 per year in Japan. The number of cases diagnosed with this may increase.
For aHUS treatment, plasma therapy such as plasma exchange and anti-C5 antibody therapy, which is a complement targeting drug, are performed. Anti-C5 antibody drugs are highly effective against aHUS, but they are expensive treatments, and a definitive diagnosis of aHUS is required before use. It is also important to decide whether to discontinue medication when remission occurs.
We have developed a plasma protein marker for aHUS, enabling differential diagnosis of aHUS and monitoring of patients during remission.
 |
Reference
- Patent pending (unpublished yet)
Principal Investigator
Noritoshi KATO (Department of Nephrology, Nagoya University Hospital)
Current Stage and Next Step
- aHUS is a designated intractable disease in Japan, and Nagoya University operates the aHUS disease office and tests many patients. This method is the result of that research.
- Differential diagnosis and remission monitoring of aHUS can be a marker/companion diagnostic for the development of complement-targeted drugs. We would like to promote collaboration between companies developing complement-targeted drugs and diagnostic drug companies.
- In the future, we plan to consider including this technology in the aHUS treatment guidelines and having it covered by insurance.
- We would also like to apply this technology to the differential diagnosis of other complement-related diseases (paroxysmal nocturnal hemoglobinuria, myasthenia gravis, neuromyelitis optica, collagen disease, etc.).
Project.BK-04011


